Surviving Gestational Diabetes: Everything I Wish I’d Known
I was devastated when I got my diagnosis of Gestational Diabetes. I cried and felt like it just wasn’t fair! However, it ended up being a blessing in disguise, and I had a very healthy baby. No one wants Gestational Diabetes, but you might as well make the best of it. Here is EVERYTHING I wish I had known – including meal and snack ideas, what to expect, and hopefully a little bit of hope.
Even though I had a feeling I might have Gestational Diabetes Mellitus (GDM) before I even took the test…it was still a hard pill to swallow.
I hoped and prayed that my one-hour Gestational Diabetes test was a false positive, but that wasn’t the case.
Throughout my journey with GDM, I learned a lot. I started this blog post and jotted down my thoughts, successes, and failures along the way.
Four weeks ago, I gave birth to a healthy baby boy. He was born three weeks early (all on his own!), and although it was a difficult journey – I can 100% say it was worth it.
I even can say that it may have been a blessing in disguise. I was healthier than ever before. I actually am at the lowest weight I’ve been at in years – and 15 pounds under my pre-pregnancy weight.
Getting any type of diagnosis during pregnancy is hard – I know I felt like it was the end of the world when I found out I had GDM.
However, learning all you can about your condition, getting appropriate medical care, and taking care of yourself can make a world of difference.
I hope that this post will help any of you that are currently going through GDM pregnancy feel a little bit better, find helpful resources, and help you get through the remainder of your pregnancy a little bit better.
If you take anything from this – have it be this.
It will be okay. Pregnancy is hard. And getting a diagnosis of Gestational Diabetes is difficult. But it will be okay.
I say this as my five-month-old is asleep next to me. I look at him and I can say with 100% certainty, “It was all worth it.” We are https://www.facebook.com/groups/405637750514880SO lucky to live in this day and time that we do – there are so many resources to help our babies get here safely – and that is a blessing in and of itself.
Please keep in mind that this is my story. My GDM was “less severe” than others, but it was still difficult to handle at times. As I will talk about – there’s a lot of conflicting advice out there, and the path I took may not be the same one you take. Nothing in this post should be taken as medical advice.
Join our New “Thriving Through Gestational Diabetes” Facebook Community!
Table of contents
[birdsend form=8194]
My Positive Gestational Diabetes Story
First, I want to share a little bit about my experience with GDM.
At 26 weeks, I took the glucose tolerance test. I found out that I had failed at a level of 177.
Although I knew there were plenty of false positives with the one-hour test…my gut told me that wasn’t the case.
In weeks previous, I had realized that sugar was making me feel really sick. I remember having some chia seed oatmeal and feeling so sick afterward – and when I looked at the nutrition and saw how much sugar was in it, I thought, “Do I have Gestational Diabetes?”
I was in Chicago at a conference at the time, and I immediately searched for a book called, “Real Food for Gestational Diabetes.” I had seen my friend, Jenn, from Plus Size Birth, do an interview with the author, Lily Nichols, a few weeks before. I don’t know why it stood out to me at the time, but now I know why.
I read the whole book in one night. At this point, I hadn’t taken the three hour test, but I had already resigned myself to having Gestational Diabetes.
It gave me hope. It helped me realize that this diagnose wasn’t necessarily because of anything I had done. It helped me come up with a plan that would allow me to have a healthy pregnancy – and a healthy baby.
A few days later, I flew to North Carolina to meet up with Forrest and the boys.
Since it would be a week before I got back to Colorado, I went and got the three hour glucose test done.
The results were sent to my doctor’s office the next morning, but I didn’t hear anything from them. I had to wait for the results to be posted on the LabCorp website a few days later, however, my OBGYN office had said that no news was good news.
On the plane, I was stuck in a middle seat on a bumpy and stuffy flight.
I was starving and nauseated, so I ate whatever I could find – which were pretty high in carbs.
I am not sure I had felt that sick my entire pregnancy – as soon as I got off the plane, I promptly threw up and felt pretty terrible. When I realized that the food I ate only made me feel worse, I once again felt like my results were going to come back with GDM.
Five days went by, and I didn’t hear anything. I got an email telling me my results were listed on the website, so I nervously opened them.
I scrolled down one line at a time.
Fasting – 65. Normal!
One hour – Normal!
And then, in red print, I saw that I failed by 2 and 3 hour test.
For some reason, I didn’t spike at all at one hour, but I did on those last two hours.
I didn’t fail by much (just a couple of points), but from my research, I knew that if you failed more than one number, I would be diagnosed with Gestational Diabetes.
As soon as I got those results, I walked up to Walgreens, purchased a blood glucose monitor and strips, and I started testing my blood sugar. I was pleasantly surprised to see my numbers were pretty normal, but I anxiously waited to hear from my doctor’s office.
They finally called to let me know that even though I was very borderline, I did fail the test, and I needed to visit with the office’s dietiain the next week.
The moment I knew I had Gestational Diabetes, I changed my diet immediately. In the past, I had tried to cut back on carbs and sugar without a lot of luck, but I felt blessed with will power beyond my own during the rest of my pregnancy to completely change my diet.
I was fortunate that my OBGYN office had a great dietian on staff who had very similar opinions to those that were in “Real Food for Gestational Diabetes.” It made it so much easier, especially as I heard about moms who weren’t quite as lucky.
I was diagnosed at about 27 weeks, and I had Andrew at 37 weeks and two days. He was 7 lbs 2.4 ounces. Ten weeks may not seem like a long time, but it felt like an eternity. This wasn’t nearly as long as some women have the diagnosis for, but it sure felt like I would never give birth.
However, the rest of my pregnancy, I ate better than I probably have in my life, and I gained a greater desire to be healthier, even after I gave birth.
It wasn’t always easy, and there were times where I just felt mad. But I am grateful for the experience and support that came from it.
And let me tell you, this moment made every poke, cookie I passed up, and frustration worth it:

My hope in writing this post is to help moms who are going through a Gestational Diabetes diagnosis feel a little less sad and a little more empowered. I want you to know that you can still have a healthy pregnancy and come out better than before. And that it’s okay to have all the emotions you are likely feeling right now!
Please do not take anything in this article as medical advice.
What Every GD Mom Should Know

Don’t Blame Yourself
I LOVE this video from Pregnancy and Postpartum TV. She specializes in Gestational Diabetes, and she explains why you shouldn’t blame yourself.

Maybe there was something you could have done differently, but honestly, a lot of the time, it’s out of your control. And there’s no use in wishing you’d changed something – all you can do is look forward!
It’s Okay to Cry
I cried when I saw those 2 and 3-hour tests pop up as over the limit.
I cried when I felt so hungry and nothing I could eat sounded good.
I cried when I saw other pregnant friends posting pictures of all the delicious foods they were eating.
I cried as I felt like I had failed my child, especially as I read about some of the issues that are at a higher risk of happening because of GDM.
It is OKAY to cry and go through a grieving process when you get diagnosed. Others may not understand what the big deal is – but it IS a big deal – even if it’s just to you.
A GDM diagnosis can be life-altering – even if it’s just for a short time. Most women have to change their lifestyle and eating habits at least a little bit with it.
Pregnancy is emotional as it is, and when you have any complications, it can feel daunting.
So don’t hold back the tears. It’s okay to cry.
Every journey is different
I joined several groups for moms who had Gestational Diabets on Facebook, and I realized what an individual issue this is.
Some women can’t even look at certain foods without spiking.
Some women can still eat pastas and fruit in moderation.
Some women have to be on medication.
Some women can be completely diet controlled.
No matter who you are here, just know that your journey will be different from others. You have to find what works for you.
I am grateful that I had a milder version of GDM – though I was really strict with my diet, so I have no idea what would have happened had I been a little more leniant. I’m grateful that I was able to be diet controlled – but I was also grateful for the moms who were on medication who showed that being on medication wasn’t a terrible thing.
At the end of the day, healthy mom and healthy baby are the ultimate goal.
The diet that I followed goes a bit against some of the current standards and recommendations (I ate between 130 and 150 carbs a day – typically recommendations are 175+. See “Real Food for Gestational Diabetes” for information on lower carb amounts, as well as research on whether or not ketones in your urine are an issue – this is something many women are concerned about when eating fewer carbs).
I felt good about this, and my body seemed to respond well. But it may not be the best for all moms. As with everything related to your body, I think it’s so important to be informed so you can make a decision that’s best ofr you.
Don’t blame yourself
When I first started researching GDM, I kept coming across articles that said sometimes there are certain factors that you put you at a higher risk for having GDM.
While I wasn’t super overweight, I wished I had lost a few more pounds before I got pregnant.
I am known to enjoy sweets, but I didn’t feel like I overdid it that much.
I tried my best to be healthy, but I struggled with really bad morning sickness – and sometimes, you just have to eat whatever you can keep down.
When I met with my dietiian, she went over all the factors for GDM and said, “You really don’t have any of these. I’m quite certain that this is just a placental issues.”
And even if I’d had every risk factor – blaming yourself does no good. You can always be healthier moving forward but you can’t change the past. Wishing you’d done something different only makes it harder.
The truth is, around 50% of GDM cases have unknown causes, and it just comes down to the placenta just not doing it’s job.
Detox
The first two weeks after I started my new lifestyle, I was exhausted and starving.
I felt like I kept eating and never being full.
My head hurt like crazy.
I already felt so worn down being pregnant, but this was at a whole new level.
I’m quite certain this was a detoxing period that often happens when you drastically change you diet – especially when you almost completely cut out sugar and cut back on carbs quite a bit.
It can feel totally miserable, but I promise, it does get better.
That feeling of always being hungry goes away, your mind will clear up, and you will start to feel a little better. I found I felt so much better after about two weeks.
So much conflicting advice
I’ve found that with most medical topics, there is almost always conflicting advice.
The truth is, a lot of the recommendations for GDM should be updated and are based on decades old research.
As I mentioned earlier, I followed a less conventional approach by using the recommendations from “Real Food for Gestational Diabetes” as well as the advice of my dietitian.
However, I know that it can be hard to go against the grain of what’s always been done, especially if your provider doesn’t agree with it.
I heard so many women who got differing opinions from their doctor, a high-risk physician, and their dietitian, which can make it even harder to know what to do!
Find a Provider You Work Well With
Pregnancy is hard enough as it is – add in a provider that you don’t exactly jive with, and it can feel nearly impossible to handle!
Make sure that you feel comfortable talking with your medical provider about your condition and that they are willing to talk through things with you.
This doesn’t mean you always have to agree on everything – but being able to have a conversation (without the idea of “my way or the highway”) is so important when you have pregnancy complications.
Get up and Walk
I don’t think I ever walked so much in my life as I did when I had GDM.
I would walk after every meal – if the weather was too hot, I would ride my stationary bike.
Toward the end of my pregnancy, I had a lot of extra pressure due to extra fluid, so walking very far was almost impossible, but I would still try to go around the block once or twice a day.
This can help your body metabolize sugars better and help with your numbers. Any kind of activity will be helpful, but I think walking is the easiest
You’ll probably think you were misdiagnosed
Here is a post I put in a Facebook group I am in shortly after I was diagnosed:
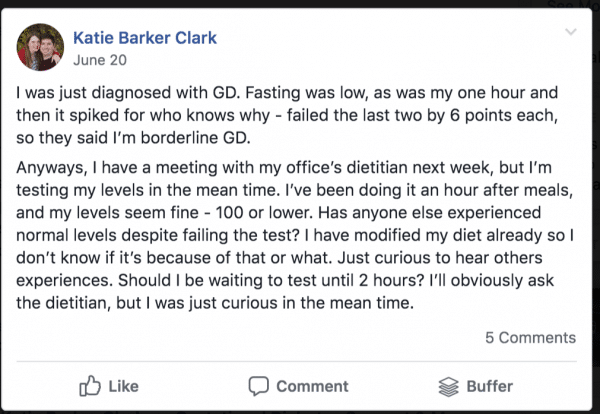
It really seemed like I had been misdiagnosed, especially when I saw my numbers compared to a lot of peoples.
I had lots of people be like, “Are you sure you have it?” I questioned it quite a bit!
I do believe I had a milder case, but it was very apparent to me if I ever cheated how terrible I felt. I didn’t cheat very often – only a couple of times – but I definitely hated how I felt.
My biggest splurge was when I ate three cookies when I was about 32 weeks pregnant. I tested my blood sugar 1.5 hours afterward, and I was at 136.
I think if I had been less careful with my food, I would have seen higher numbers. But I definitely think I was most sensitive to sugar.
Anyways! As I spent more time in that group, I think every day I saw a post come up where someone felt like they were misdiagnosed.
I’m sure you can be misdiagnosed, but it’s not super common. But it is common to wonder if you were 🙂
Many women see their GDM get worse the further along in their pregnancy they get, so it’s definitely possible to have good numbers that progressively get worse.
It is not a death sentence
It is easy to feel like this will be your life forever and that it’s the end of the world.
I promise, it’s not. And your pregnancy WILL eventually end.
Most of our lives revolve around eating. There’s food at just about every social function. And it can be hard to totally change the way you eat and associate with others.
But it will be okay. I learned that I actually have quite a bit of self-control, and that life went on even if I had to forego some ice cream at a church event.
It’s okay to experiment with foods
Not everyone reacts to foods the same way with Gestational Diabetes.
I was generally okay with most fruits – but many women are not (especially in the morning).
If you are trying out a food that might be considered borderline, just try it and see how your blood sugar does.
You May Not Require Extra Monitoring

In one of the groups I was in, I noticed that everyone seemed to have a lot of extra monitoring – ultrasounds every other week, non-stress tests weekly, etc.
My office was treating my pregnancy pretty normal – I had an extra ultrasound at 28 weeks and 35 weeks (and the 28 week one was scheduled before I even had GDM, since they wanted to make sure I wasn’t having another IUGR baby). But they didn’t really mention much – all I did was send my numbers to my dietican each week, and that was that.
I was worried that they weren’t monitoring me close enough – but as I talked with other moms, I wasn’t alone.
I was diet-controlled, and while Andrew was measuring about 1-2 weeks head, there wasn’t a cause for control. When I was 37 weeks, they said I would need to start coming in for non-stress tests at that point – but then I had Andrew the next day, so that never happened.
The one time I was monitored (in the picture above) was because my baby’s heart rate was a little high. Not GDM related!
Some people do require more monitoring – but don’t worry if you don’t. It likely just means that your numbers are good and the baby looks good!
Medication isn’t the end of the world
In an ideal world, everyone would have their GDM managed by diet alone.
But that doesn’t always happen. Even people who try their very hardest may end up on insulin or some other kind of medication – it doesn’t mean you failed or did something wrong.
Medication exists to help our babies get here as safe as possible, so if there comes a point in your pregnancy where you might need medication…that is okay! It exists for a reason, and that reason is to help you and baby be as healthy as possible.
It might be the best thing that happened to me
I know, that sounds crazy. And that is the LAST thing I would have ever thought I’d say when I was diagnosed.
But it was a wake up call to me. I am now 7.5 months postpartum, and I weigh 30 pounds less than I did when I got pregnant. I learned how to eat better, listen to my body, and take care of myself. I realized that this was my chance to get healthy and give myself a better chance at avoiding certain health issues.
GDM Complications
There are some complications that can come with Gestational Diabetes. Keep in mind that just because these happen sometimes doesn’t mean they will happen to you.
Often, the best prevention for these is getting your Gestational Diabetes under control.
- A big baby – because of the extra glucose, they can be larger. Andrew was measuring large, but as soon as I got my blood sugar under control, he wasn’t growing as rapidly as he was before
- Shoulder Dystocia
- Polyhydraminos – I actually had mild polyhydraminos. But with my past pregnancies, I had a lot of fluid, too. My mom did as well! My doctors didn’t feel mine was attributed to GDM, since it was so well-controlled. When he was born, though, my doctor said she’d never seen so much fluid!
- Preterm birth
- Erratic blood sugar for the baby after birth
- Type 2 Diabetes later in life
- High blood pressure
Getting Started with Monitoring
Glucose Monitor
There are a lot of glucose monitors out there. Most insurances should cover the monitor and testing strips – though they don’t always cover everything that you need.
Because I was self-pay, I just bought one at Walgreens. It seemed to work pretty well, and I didn’t see any complaints against it in the group I was in. It was called True Metrix
The one monitor I saw people consistnetly complaining about having false high numbers is the One Touch monitor. It’s actually the one my office used, and once they took my blood with it there, and it was SO much higher than I ever got with my monitor.
All monitors have a range of accuracy, but if it’s giving false high numbers, that is a problem. My fasting was right on with what it was in my blood test, and there was no reason to believe it was inaccurate otherwise.
A lot of people seem to like the Contour Next One or the Reli On. Here is a great article about the accuracy of different blood glucose monitors.
Buy supplies online
If you don’t think your insurance will cover everything (specifically the strips), make sure to get one that you can find the supplies for at an affordable price.
I ended up getting all my strips on Amazon for WAY less than it would have cost to go through the pharmacy or over the counter at Walgreens.
Amazon often has test strips for the more popular brands, so definitely look into that.
When Should you test?
There is always a lot of debate about if you should test one hour after you eat or two hours.
I was instructed to test one hour after – but I would occasionally check after two hours just to make sure I wasn’t spiking later. With my glucose test, I didn’t spike until hours 2 and 3. But my numbers always were lower after two hours.
So don’t get confused if you see other people testing at a different time than you. Just do what your doctor says.
Set a timer
I would almost always forget when I ate and I would start to second-guess of when I should be testing.
So it was helpful to set a timer so I would always know when I was supposed to test. As soon as I took a bite, I would set a timer for one hour later.
App
There are tons of ways you can keep track of your numbers and your meals.
A lot of dietians will give you a paper where you can write everything done, but I felt like this would be too hard to keep track of.
So I used mobile apps! For tracking my food, I used My Fitness Pal. I had already used this for many years, so I was pretty familiar with it.
You can set macro-based goals (protein, fat, and carbs) with a paid plan. They have a HUGE database of foods, and even if they don’t, you can easily add in the calories.
I religiously tracked every single thing I ate in My Fitness Pal while I was pregnant so I knew that I was eating enough of the right foods.
I also downloaded an app to track my numbers. There are tons of them out there, and I used Sugar Sense. To be honest, it was a bit glitchy at times!
Lancets
This was another one of those controversial topics. Whether or not you should use the same Lancet or not.
I read a lot and a lot of diabetes forums had people say that they did not change their lancet every time they tested.
However some people are adamant that you do. Just another thing to talk to your doctor about.
Favorite Meals and Recipes
I wish I had been better at writing down all of my favorite recipes, but I did have a few I jotted down.
I also thought I would share my MyFitnessPal food diary. You will need to use the code GDM to access it – and it’s from about June 2019 through September 2019. It might give you some ideas.
I also found a lot of great ideas in the Clean Simple Eats cookbooks. All of these recipes fit very well within my allotted goals. They give the carbs, fat, and protein for all the recipes, and there are lots of ideas for breakfast, lunch, dinner and desserts.
Be sure to signup below for my FREE Gestational Diabetes cheat sheet + a TON of snack ideas that you can make. It’s actually taken from the cookbook above, so if you are trying to decide if you want it, be sure to sign up!
[birdsend form=8194]
- Eggs with bacon bites, mozzarella, and veggies. I just ate a lot of eggs in general. It took me months to be able to eat them again after I had my baby.
- Corn tortilla with chicken, Greek yogurt, cheese, salsa, refried beans and spinach
- Protein Pasta with meat sauce
- Sandwich thin with hamburger patty, ketchup, mustard
- Oatmeal with protein powder and sausage kink
- Just crack an egg cups
- Naan pizzas
- BBQ chicken on sandwich thin
- Costco Chicken Salad
Favorite Snacks/Treats
Favorite Foods I found
There are a lot of different foods and brands I tried while I was pregnant. Some were duds, and some I loved.
I discovered that I REALLY didn’t like anything with monk fruit or swerve. It just had a weird after taste. I also avoided anything with splenda/sucralose.
This list is not all encompassing, but these were some of my favorite foods I found throughout my GDM journey. You can check out even more on my Gestational Diabetes food list.
A great place to buy a lot of these items (and others) is Thrive Market.
- Banza Pasta – high protein. I would serve with a lower sugar pasta sauce and ground beef and LOTS of veggies on the side
- Smoothies
- Whole wheat ritz with summe sausage and tomatoes
- Berries
- Built bars – you can get 10% off with the code CLARKS. This are the best protein bars I have found, and they quickly started tasting like a candy bar. Great macros!
- Rip van Wafels – I actually discovered these after my pregnancy, but I WISH I known about them. Low carbs and sugar. They even have a protein version. Use code CLARKS for 10% off. These really are a treat!
- Costco rotisserie chicken
- Nature Valley Protein Bars
- Sandwich thins
- Low cow fudge bars (Kroger)
- Halo top pops
- Triple zero oikos
- Whole wheat Toast with PB
- Jerky
- Apple with almond butter
Gestational Diabetes Diet Tips
How to Measure Food
There are various ways to measure your food. My dietician gave me a guide for measuring food that was based on your hand – but I was a little crazy and wanted to make sure I knew EXACTLY what I was taking in.
I strongly recommend buying an accurate food scale.
Find your favorites and repeat
I’m someone who really likes to have a variety of recipes on our family’s meal plan – and I don’t repeat things super often.
However, when I was pregnant, that was different. Once I found meals that worked well with my numbers, and that I enjoyed…we repeated them. This was especially the case for breakfast and lunch!
Leftovers
I did not love leftovers until I got GDM – and then I realized how much easier it made my life if I ate a “safe” meal from the night before for lunch the next day.
There are good and bad ways to do leftovers. I highly recommend reheating things in the oven or stovetop if you can. Add fresh cheese to things. Make sure it’s heated all the way through.
And invest in good storage containers!
Keep it Simple
Don’t over plan or overcook (unless you want to!). For me, the key to success was keeping everything as simple as possible.
1/2 your plate veggies
I think this is good advice for everyone, but it really helped me when I was trying to put my plate together.
Throw in veggies any chance you get
I always have a hard time getting vegetables in my diet, but I made a big effort to change that when I was pregnant.
I always had spinach, chopped up onions and peppers, baby tomatoes, etc. that I could throw into casseroles, eggs, or make a quick salad. The more veggies you can get in your diet, the better!
Mentally prep for gatherings
The hardest thing for me was when I went to church or family gatherings. If I mentally prepared myself and brought my own “safe” food, it was easier.
But when I didn’t, I would sit there and just feel sad as I watched everyone make ice cream sundaes
Eating Out
I love to go out to eat, but I have to admit it was considerably less fun once I was diagnosed with GDM.
My options often seemed limited to a piece of meat and vegetables. I would sometimes let myself have a small piece of bread with butter (if the restaurant offered it), and I could handle that pretty well.
One recommendation I have is to always check nutrition facts before you go out. That way you can make an informed decision and plan on what you are going to order before you go.
Here are some of my favorite things I would get:
- Chick-fil-A nuggets with a side salad
- Domino’s Thin Crust Pizza with veggies and sausage or pepperoni
- Taco Bell crunchy beef tacos
- Salads of all kinds – watch the dressing – some dressings can be filled with carbs!
- Longhorn Steakhouse Parmesan crusted chicken with broccoli
- Wendy’s chili and a side salad
- Chicken nuggets at pretty much any fast food place
- Hamburgers with no bun or half the bun (check the calories beforehand).
Resources I found Helpful
The best thing you can do is manage your Gestational Diabetes as well as you can. This requires working with your doctor/midwife and usually a diabetes counselor.
I have a lot of feelings on some of the recommendations given to mothers with Gestational Diabetes, but I would just encourage you to do your research and work with a trusted care provider to come up with the best course of action.
The following resources were very helpful to me during my pregnancy:
- Anything from Lily Nichols. She is the author of “Real Food for Pregnancy” and “Real Food for Gestational Diabetes“. I learned about her about a month before I got diagnosed with GDM, and as soon as I got the results, I downloaded the eBook “Real Food for Gestational Diabetes” and read it in one sitting. Her advice is different from mainstream information, but I believe it’s why I have had such a healthy pregnancy and postpartum. Her book is amazing, but you should also follow her on Instagram, check out her website, and even consider taking her course for pregnant moms with GDM.
- Jessica from Pregnancy and Postpartum TV and Pregnancy and Childhood Nutrition. She has wonderful workouts, a great Facebook support group, and a lot of very helpful information for GDM.
- My friend, Amberly, wrote this great post that I referenced a lot during my pregnancy. It gave me a lot of hope!
What to Expect During Labor and After Pregnancy
While you are in labor, they will check your blood sugar at some point. They definitely have a note that you have GD, but I didn’t notice any differences.
Honestly, just be prepared for child birth! I highly recommend The Online Prenatal Class for Couples. It has SO much good information and helps prepare you as best you can. It’s taught by a very experienced labor and delivery nurse. You can get 10% off with the code CLARKS. I just talked to her, and she said, “Gestational diabetes isn’t as rare as you might think and I will share some things to watch out for as you traverse your pregnancy journey.”
After you give birth, they may check yours again – they never checked mine. However, they will carefully monitor your baby’s blood sugar.
This was the most stressful thing for me, because the bedside monitor was showing Andrew a little low, but when they would do a lab verify, his levels were fine. I couldn’t feed him on demand, and it was just really stressful.
I found out later that his levels – even on a bedside monitor – were actually acceptable. However, one nurse noted that she saw his lip quiver once, deemed his as symptomatic, and the acceptable levels changed. Shaking is a sign of low blood sugar, but it’s typically their whole body. Andrew’s lip quivered randomly until he was about three months old – more likely just due to an immature nervous system.
Anyways! They will check them starting about two hours after birth. I believe they have to get four acceptable blood sugar levels before they’ll stop testing – and they generally can stop altogether at 24 hours after birth.
If your baby does have true blood sugar levels, you may have to supplement. I go over all of this in this post – Gestational Diabetes and Breastfeeding. I highly recommend reading it.
The most important thing is to be informed and know what’s going to happen.
Generally, your blood sugars will stabilize pretty soon after birth, though for some women it may take a few months. You will be given a blood glucose challenge at around six weeks – though my office let me just get an a1C done.
Future Pregnancies
You are more likely to develop Gestational Diabetes in subsequent pregnancies. There is between a 45 and 65 percent chance.
According to Everyday Health, here are some factors that may increase your chance of developing it again:
- Race. Gestational diabetes is more common in African-Americans, American Indians, Asian-Americans, and Hispanic Americans.
- Number of pregnancies. The risk of recurrent gestational diabetes increases with the number of pregnancies you have.
- Insulin. If you needed insulin to control your sugar during your first pregnancy, your risk of gestational diabetes is higher.
- Your baby’s weight. If your first baby was overly large at birth, you are more likely to have gestational diabetes in the future.
- Your weight. If you are overweight, especially if you weigh over 190 pounds before your pregnancy, you are at higher risk for recurrent gestational diabetes. Your risk may also be increased if you gain weight between pregnancies or if you eat a high-fat diet.
It’s hard to say if you for sure will. But post-pregnancy, it can be super helpful to get and stay healthy. While you may still get GD again, it may lessen the likelihood.
As I’ve mentioned, GDM ended up being a big blessing in disguise. I am healthier than I probably ever have been. I’m down 30 pounds from my pre-pregnancy weight (though some of that is due to Intermittent Fasting). I learned how to take care of myself, love to exercise, and I realized how much better I feel when I do.
Gestational Diabetes can be a frustrating and overwhelming diagnosis. It’s okay to scared and sad and all other kinds of emotions. However, I hope that this post can bring you some hope. Please let me know if you have any questions, I’d love to help you in any way I can.




I needed this! I haven’t technically been diagnosed with GD. My midwives take a different approach and I just monitor my blood sugar for a little while and take note. It started out very interesting but as I continue to test I find more and more that I cannot eat and it definitely feels frustrating. I’ve also read real foods for GD which I loved. When you said it’s ok to cry because you’re hungry and nothing you can have sounds good, that resonated with me.
Anyway, thank you for this article!
I was just Diagnosed with Gestational Diabetes and your article was the first one to pop up when I started researching. I believe it was God send. This was everything I needed to hear and reaffirm that it’s going to be okay. Thank you so much for sharing your experience!!
Shantel- Blog-“ A Picture Worth Style”
I’m so glad! Best of luck with your pregnancy.
I feel this same way. I keep crying and I’m super emotional about it & I just feel understood. I thank you!
Love this article, just found out I have gestational diabetes. Have been struggling coming to terms with it. Great article to read gave me reassurance that the gestational diabetes journey is going to be okay.
Just like to say thank you for putting it out there.
I am glad it was helpful! Best of luck with your pregnancy!
I’ve been lucky enough not to get gestational diabetes with any of my pregnancies, but I know people who have had it and it’s been a real struggle! I’ll definitely pass this on!